The U.S. healthcare market is undergoing a confluence of changes, which is redefining the industry and altering the way its associated institutions do business.
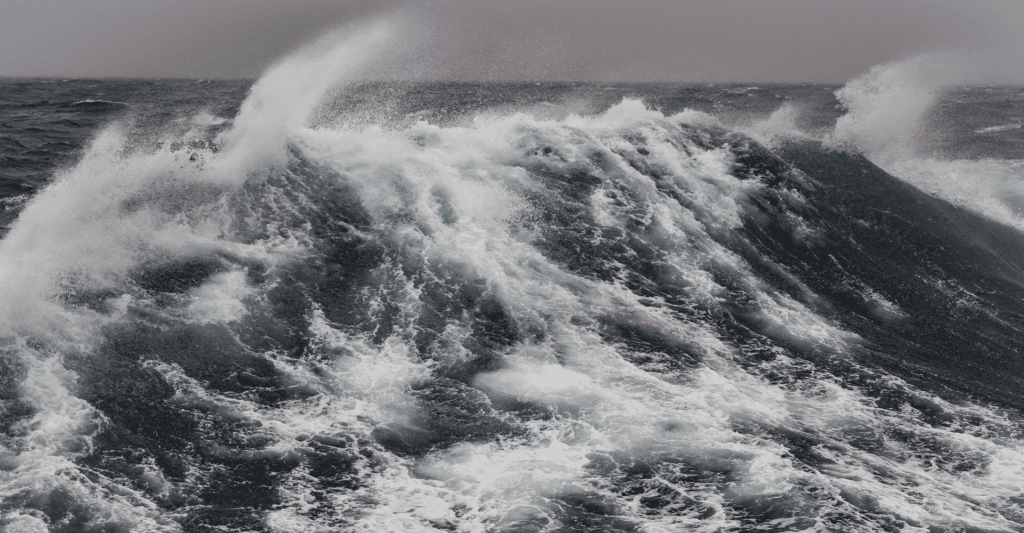
The result is essentially a new model for the nation’s healthcare system. It’s a “perfect storm” with care and cost at its center. How has this happened? And what are the implications for how hospitals will proceed?
The changes will be impacted by—and, in turn, impact—hospitals’ internal leaders as well as external vendors—from primary ones like electronic health record (EHR) companies to secondary ones such as suppliers of patient engagement tools. To better understand what exactly is happening and why, let’s look at a few influential factors at play here:
- Mergers & Acquisitions: According to a new Kaufman, Hall & Associates report, the number of hospital mergers and acquisitions in 2017 was the highest it has been this century and nearly double what it was 10 years ago and 13% over 2016 activity. 2017 was a “transformative year,” according to the report.
For hospitals, this means unprecedented, disruptive change integrating multiple care and cost systems. As one hospital system’s chief medical information officer put it, “This is so radical, it’s effectively put a freeze on all else but the integration. This will inform and, in most cases, override most of what we do except direct care for the next 24 months minimum.”
- Compliance & penalties: At the same time, the Centers for Medicare and Medicaid Services (CMS), the nation’s primary payer, has increased its care cost and quality penalties and altered how reimbursements, incentives and benchmarks for compliance are handled. For example, in 2012 the agency began levying penalties for hospital readmissions. In 2015, it changed the focus for Meaningful Use2 demanding even more. EHR incentive program requirements now require “advanced use of certified EHR technology to support health information exchange and interoperability, advanced quality measurement, and maximizing clinical effectiveness and efficiencies.” CMS, as we know, leads the way on policy and all other major payers tend to follow.
- Reimbursements tied to episodes, Not Hospital Stays: Contributing to this sea change, CMS essentially renamed what it pays for: the episode—with ramifications starting before a patient is even admitted to the hospital and continuing through well after they are discharged. This is the new CMS economy—i.e., what it will pay for or not pay for. This sharing of cost among providers throughout the care continuum is a smart move for CMS and, in theory, good for patients too, if it’s acted upon—and there are signs that it will be. It’s also good for hospitals—surprisingly, perhaps, as it means hospital leaders will have a longer period of responsibility for their patients. If done well, they can “meet” patients long before hospital admission and, in so doing, improve much more than just satisfaction and reputation.
- The “wait-and-see” freeze: Rounding out this perfect storm is the stalling effect of a “wait-and-see” phenomenon resulting, in part, from the uncertainty of the current political climate and the unpredictability around healthcare regulations, programs, grants and research (even that which has been “funded” and is presumably secure). These are now being re-examined and delayed, if not canceled outright. In short, U.S. healthcare is experiencing integration exhaustion.
This has led to a halting of many commitments to improving efficiencies in hospital care and cost. As this trickles down to the department level, clinical and marketing teams have stopped initiatives already in progress and, in some cases, even reverted back to old ways of doing things, despite knowing these approaches are less effective and will not improve care or cost. U.S. healthcare is hardwired to focus on care and minimize risk, as it should be. But a new acumen—knowledge, skills and time to implement and integrate digital solutions, while also managing mounting financial concerns—is required for today’s hospital leaders.
Much of this is not intuitive to this market segment. It marks huge changes for all, particularly those in clinical or marketing roles.
- EHRs and other primary vendors become equal partners: For the first time, hospitals have dependencies on—and, therefore, are focusing on—those who are providing them with digital platforms and integration of care, safety, security and cost solutions. The buyer is the hospital, but the successful implementation requires far more work with primary vendors (Epic, Cerner and others), as well as with other vendors charged with meeting different, yet associated goals.
This is an upheaval for vendors, hospitals and physicians alike. Typical of this situation, as one hospital executive noted, “90% of contracts accepted in 2015 or 2016 have been put on hold, changed or cancelled while we update Epic.” And to the point that vendors (large and small) also are not immune to these changes, a senior VP of sales and business development, said, “We used to sell directly to the hospitals. Now there are so many layers and primary vendors it is hard to get into new places. We’ll keep our current clients and grow with them. But new business, even in new products and services in the pipeline, has been stalled or delayed.” T
- The Care-Cost Helix Both internal and external players, and the opportunities they want to champion, must speak to and focus on both sides of the care-cost continuum. Improvements in care or cost alone will not “sell.”
Understanding that the connection between care and cost is dynamic and that each is dependent upon the other is now crucial. Visualize it as a helix, “an object having a three-dimensional shape like that of a wire wound uniformly in a single layer around a cylinder or cone, as in a corkscrew or spiral staircase.” 4 on one side, the outside “wire” is care, and on the other side it is cost. The internal pieces, which keep the two sides connected, are the activities that make up the care and create the cost.
All of these pieces impact how the helix moves and twists. When one side changes, consequently, so does the other. This understanding that care and cost are inextricably interconnected helps both internal and external players identify opportunities and capitalize on them. Thinking about the continuum this way acknowledges that effective products and services help to stabilize and improve the care-cost helix. When we accept that this is one, not two separate areas of work, we talk in different terms and are open to new and different ways of leveraging what is already there in order to succeed in this new environment. It’s in this moving care-cost helix that primary vendors and secondary vendors, as well as hospital leaders, must find ways to work more effectively as one when it comes to implementation and integration. Where We Go From Here Just as hospitals are hardwired to improve care and reduce risk and cost, we in this country are wired to find opportunities in change and challenge.
And there are opportunities in the midst of this perfect storm in U.S. healthcare. However, for both internal and external players, capitalizing on them requires rethinking how to succeed in what you want to achieve. Here are a few strategies to keep in mind while navigating through this unprecedented time:
- Focus on small, but compelling successes. Pursue discreet, specific solutions that directly impact particular hospital pain points (again read: cost) in quantifiable ways. These efforts must yield short-term gains, while also showing a clear path to long-term value. And, remember, this must be for the entire care-cost helix, not just cost or just care.
- Prove it. Whether they are internal, external or a combination of both, hospital solutions are increasingly required to show immediate proof of value and effectiveness, as well as ease of integration with existing systems (think interoperability). Now, part of this proof often involves systematic patient-reported feedback (PRF) that supports the positive impact. (This feedback is not yet a requirement, but likely soon will be). For real proof of efficacy of any care-cost solution, one must start with baseline data (specific numbers). For example, what has this pain point cost the hospital over the last year? Pick a pain point that can be remedied. But know that this will not fly unless the outcome, workflow or practice that the solution will improve is simple, clear, immediate and touches the buyer’s pain point.
- Innovate on what’s already implemented. Offers of “new” initiatives, particularly if the “new” has a big price tag, will be non-starters. Instead, find opportunities to integrate with and enhance existing systems and resources that are already in place. Again, quantifiable gains are a must. This is today’s reality, both internally within hospitals and externally for vendors. The bottom line hospital leaders must now urgently attend to the interaction between their hardwired focus on care and their newly necessitated focus on cost as the driver for all they do. Overwhelming implementation and integration challenges aimed at addressing the care-cost focus caused the current freeze in decision-making and commitments.
Both internally in hospitals and externally for vendors, this has led to the need to redefine, “What’s going on here?” and “How do we fit in this new environment?” Because this sea change in U.S. healthcare has happened due to the confluence of evolving factors, there are new needs, new terms, new solutions—many of which involve digital technologies. To meet these challenges and to capitalize on the opportunities that flow from them, both internal and external players must change, too. That starts with understanding and acting on the new reality that we are all responsible for care and cost. That is how we “make us all better.”
Betsy Weaver is CEO/president and founder of TPR Media (UbiCare).
Favorite